Robotic pancreatic surgery in a high-volume pancreatic cancer surgery center – first experience
Martin Loveček Orcid.org 1, Pavel Skalický1, Dušan Klos1
+ Affiliation
Summary
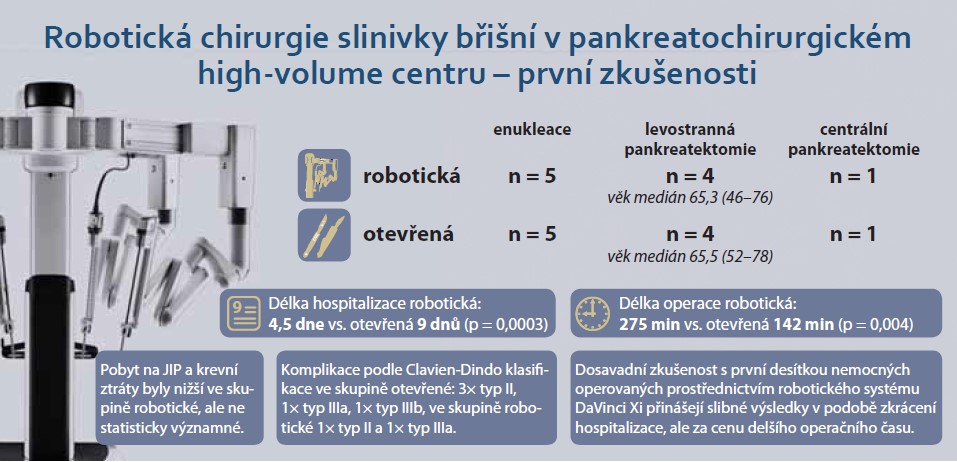
Introduction: Robotic pancreatic surgery is still not widely used in the Czech Republic. On a global scale, it is gradually being systematically implemented, especially in high-volume centers. The study presents the first experiences with robotic pancreatic surgery in a pancreatic surgery high-volume center in the Czech Republic. Methods: Comparative analysis of the first ten patients operated on robotically for pancreatic pathology with a comparable group operated open (smaller procedures: left pancreatectomy with/without splenectomy, enucleation, central resection) evaluates age, length of hospitalization, ICU stay, blood loss and operative time using non-parametric Mann--Whitney U-test, and complications and rehospitalization using descriptive statistics. The results: The compared sets consist of 10 patients, 5 women, with a robotic procedure (5× enucleation, 4× distal pancreatectomy and central resection – median age 65.3 [46–76] years) and 10 patients, 5 women, with comparable open procedures (5× enucleation, 4× distal resection and central resection – median age 65.5 [52–78]years. Hospitalization length 4.5 days vs. 9 days (P = 0.0003) and operation time 275 min vs. 142 min (P = 0.004) were statistically different in the robotic vs open group. ICU stay and blood loss were lower in the robotic group, but not statistically significant, age was comparable. Complications according to the Clavien-Dindo classification in the open group: 3× type II, 1× type IIIa, 1× type IIIb, in the robotic group 1× type II and 1× type IIIa. Rehospitalization in the open group was 2×, in the robotic group 1x, always for late postoperative complications. Conclusion: Robotic surgery of the pancreas is currently in its infancy in the Czech Republic. The experience so far with the first ten patients operated on using the DaVinci Xi robotic system has yielded promising results in form of shorter hospitalization, but at cost of longer operating time.
Keywords
pankreatektomie, enucleation, pancreas, robotics, minimal invasiveness, hospital stay, enhanced postsurgical recovery
To read this article in full, please register for free on this website.
Benefits for subscribers
Benefits for logged users
Literature
1. Jaroščiaková S, Tvrdoň J, Hladík P et al. Robotic distal pancreatectomy – the first experience. Rozhl Chir 2023; 102(3): 125–129. doi: 10.33699/PIS.2023.102.3.125-129.
2. Nickel F, Wise P, Müller PC et al. Short-term Outcomes of Robotic Versus Open Pancreatoduodenectomy – Propensity Score-matched Analysis. Ann Surg 2023; Jul 3. doi: 10.1097/SLA.0000000000005981.
3. Roesel R, Bernardi L, Bonino MA et al. Minimally-invasive versus open pancreatic enucleation: systematic review and metanalysis of short-term outcomes. HPB (Oxford) 2023; 25(6): 603–613. doi: 10.1016/j.hpb.2023.02.014.
4. Giuliani T, Perri G, Kang R et al. Current perioperative care in pancreatoduodenectomy: a step-by-step surgical roadmap from firts visit to discharge. Cancers 2023; 15(9): 2499. doi: 10.3390/cancers15092499.
5. Melloul E, Lassen K, Roulin D et al. Guidelines for Perioperative Care for Pancreatoduodenectomy: Enhanced Recovery After Surgery (ERAS) Recommendations 2019. World J Surg 2020; 44(7): 2056–2084 (2020). doi: 10.1007/s00268-020-05462-w.
6. Royall NA, Walsh RM. Robotic distal pancreatectomy and splenectomy: rationale and technical considerations. J Vis Surg 2017; 3: 135. doi: 10.21037/jovs.2017.08.01.
7. Portál ukazatelů kvality zdravotních služeb hrazených ze zdravotního pojištění. 2022 [online]. Dostupné z: https: //puk.kzp.cz.
8. Glatz T, Brinkmann S, Thaher O et al. Robotic pancreatic surgery – learning curve and implementation. Zentralbl Chir 2022; 147(2): 188–195. doi: 10.1055/a-1750-9779.
9. Nikov A, Záruba P, Ryska M et al. Miniinvazivní pankreatická resekce ve světle důkazů – state of the art. Rozhl Chir 2021; 100: 213–217. doi: 10.33699/PIS.2021.100.5.213–217.
10. Rompianesi G, Montalti R, Giglio MC et al. Robotic central pancreatexctomy: a systematic review and meta-analysis. HPB 2022; 24(2): 143–151. doi: 10.1016/j.hpb.2021.09.014.
11. Magistri P, Bobbi U, Esposito A et al. Robotic vs open distal pancreatectomy: A multi-instutional matched comparison analysis. J Hepatobiliary Pancreat Sci 2021; 28(12): 1098–1106. doi: 10.1002/jhbp.881.
12. Lof S, van der Heijde N, Abuawwad M et al. Robotic versus laparoscopic distal pancreatectomy: multicenter analysis. Br J Surg 2021; 108(2): 188–195. doi: 10.1093/bjs/znaa039.
13. van Hilst J, de Rooij T, Bosscha K et al. Laparoscopic versus open pancreatoduodenectomy for pancreatic or periampullary tumours (LEOPARD-2): a multicentre, patient-blinded, randomised controlled phase 2/3 trial. Lancet Gastroenterol Hepatol 2019; 4: 199–207. doi: 10.1016/S2468-1253(19)30004-4.
14. Strobel O, Buchler MW. Laparoscopic pancreatoduodenectomy: safety concerns and no benefits. Lancet Gastroenterol Hepatol 2019; 4(3): 186–187. doi: 10.1016/S2468-1253(19)30006-8.
15. Napoli N, kauffmann EK, Vistoli F et al. State of the art of robotic pancreatoduodenectomy. Updates in Surgery 2021; 73(3): 873–880. doi: 10.1007/s13304-021-01058-8.
16. Xourafas D, Pawlik TM, Cloyd JM. Independent predictors of increased operative time and hospital length of stay are consistent across diferent surgical approaches to pancreatoduodenectomy. J GastrointestSurg 2018; 22(11): 1911–1919. doi: 10.1007/s11605-018-3834-6.
17. Liu R, Zhang T, Zhao ZM et al. The surgical outcomes of robot-assisted laparoscopic pancreaticoduodenectomy versus laparoscopic pancreaticoduodenectomy for periampullary neoplasms: a comparative study of a single center. Surg Endosc 2017; 31(6): 2380–2386. doi: 10.1007/s00464-016-5238-6.
18. Nassour I, Wang SC, Porembka MR et al. Robotic versus laparoscopic pancreaticoduodenectomy: a NSQIP analysis. J Gastrointest Surg 2017; 21(11): 1784–1792. doi: 10.1007/s11605-017-3543-6.
19. Nassour I, Choti MA, Porembka MR et al. Robotic-assisted versus laparoscopic pancreaticoduodenectomy: oncological outcomes. Surg Endosc 2018; 32(6): 2907– 2913. doi: 10.1007/s00 464-017-6002-2.'
20. Zimmerman AM, Roye DG, Charpentier KP. A comparison of outcomes between open, laparoscopic and robotic pancreaticoduodenectomy. HPB (Oxford) 2018; 20(4): 364–369. doi: 10.1016/j.hpb.2017.10.008.
21. Lof S, Claassen L, Hannink G et al. Learning curves of minimally invasive distal pancreatectomy in experienced pancreatic centers. JAMA Surg 2023; e232279. doi: 10.1001/jamasurg. 2023.2279.