Inflammatory bowel disease has a negative impact on patients reproductive behaviour: the first multicentre survey in the Czech Republic
Dana Ďuricová1,2, Zuzana Krátká3, Martin Bortlík4, Lenka Slabá5, Kristýna Strnadová3, Tereza Kovářová3, Milan Lukáš Orcid.org 1, Martina Pfeiferová5
+ Affiliation
Summary
Background:
Several previous studies reported the negative impact of inflammatory bowel disease (IBD) on reproductive plans and fertility rate. The aim of our study was to investigate, for the first time, reproductive attitudes and fertility rate among Czech patients with IBD.
Methods:
Between March and August 2019, consecutive patients with IBD from 22 centres across the Czech Republic responded anonymously to a predefined questionnaire focused on the patients’ demographics, details of IBD and treatment, gynaecological/urological history, reproductive issues and patients’ knowledge on this topic.
Results:
The questionnaire was filled in by 798 patients (526 women; median age 34 years, 66% with Crohn’s disease). Of these, 58% of the females and 47.1% of the males already had ≥ 1 child (median 2 children). Women with IBD were significantly more worried about infertility (55.5% versus 22.4%), had more limitations in their sexual life (53.2% vs. 26.8%) and more frequently changed their earlier reproductive plans (27.6% versus 11.0%) than the males (p < 0.0001). The total fertility rate in female IBD patients was lower compared to the general population with 1.004 live births/IBD woman versus 1.69 live births/woman in the Czech population. The pattern of decreased fertility was observed in all age-specific categories. Of the childless patients, 14% of the women and 18.1% of the men were voluntarily childless. Approximately one-half of them indicated their IBD to be the primary cause.
Conclusions:
IBD seems to have a negative impact on patients’ reproductive plans and attitudes. The fertility rate in Czech IBD female patients was decreased compared to the general population in this study.
Keywords
inflammatory bowel disease, fertility, reproduction
Introduction
Inflammatory bowel diseases (IBD) are diagnosed mainly in adolescents and young adults, thus affecting the childbearing period of human life [1]. This fact may have a fundamental impact on the reproductive behaviour of patients and their family planning decisions. Although fertility in non-operated IBD patients in remission is considered similar to the background population, a higher rate of voluntary childlessness has been reported among individuals with IBD [2–4]. The most commonly reported reasons for voluntary childlessness were concerns regarding disease heritability, fear of the negative impact of IBD on pregnancy outcome or vice versa and concerns regarding the safety of medication [5–7]. Importantly, poor patient knowledge on this topic has been shown to be associated with negative reproductive views and voluntary childlessness, emphasizing the importance of patient education [8,9].
So far, most of the studies published in this field have been conducted in North America, Australia or the United Kingdom, with only a few in other European countries and none in Central or Eastern Europe.
Therefore, the aim of our study initiated by the Patient Organisation ‘Pacienti IBD z.s.’ was to investigate for the first time several aspects of the reproductive behaviour of patients with IBD in the Czech Republic. Specifically, we studied i) the impact of the disease on patients’ reproductive behaviour and attitudes; ii) the fertility rate in women with IBD; and iii) some areas of patients’ disease-specific reproductive knowledge.
Materials and Methods
Between March and August 2019 consecutive patients with IBD (women aged 18–55 years and men aged 18–65 years), irrespective of disease type or disease activity, were surveyed anonymously using a predefined questionnaire. The majority of the patients were recruited during their scheduled visit to a gastroenterology centre. In total, 22 centres across the Czech Republic participated in the study. The rest of the individuals were addressed via a newsletter of Patient Organisation and participated in an online survey using a web application placed on the website of Patient Organisation.
Data collection
Two versions of the questionnaire, one for male and one for female patients, were created by physicians at 2 participating centres and commented upon by members of Patient Organisation. In total, the female questionnaire contained 52 and the male, 44 questions. The questionnaire was divided into 5 sections focused on the patients’ demographics, details of IBD and treatment, gynaecological/urological history, reproductive issues and patients’ knowledge on this topic. In the ‘reproductive issue’ section the patients were asked about their former reproductive plans and the impact of the disease on them, fears regarding infertility, number of children, their timing with respect to IBD, conception planning, reasons for childlessness and experience with infertility treatment. Most of the questions (75% and 89% for the female and male versions, respectively) were identical for both forms of the questionnaire. Over 90% of the questions were constructed as a multiple-choice ‘check-box’ with some of the options requiring an additional free text response. This article reports only the most relevant results of the survey.
Fertility rate
The total fertility rate was calculated as the mean number of children per woman with a known number of children. Since the age distribution of IBD women did not represent the age distribution of women from the general Czech population, we further calculated age-specific cohort fertility. The data on the fertility rate were compared with the data on population fertility obtained from the Czech Statistical Institute [10].
Statistical analysis
Categorical data were described as absolute number and percentage, quantitative data as median and range. The chi-square test was used for the comparison of categorical data while the Mann-Whitney test was used for quantitative data. Logistic regression analysis was performed to assess the impact of several clinical factors (type of IBD, history of bowel surgery, relapse frequency and ever use of biologics) on reproduction outcomes. All variables with a p-value < 0.1 were then included into a multivariate model. The impact of several potential factors adjusted by age (education, type of IBD, previous bowel surgery, ever use of biological therapy, relapse frequency and perianal disease in Crohn’s disease) on female fertility were analysed using a linear regression model with ß regression coefficient and 95% confidence interval (CI). A p-value < 0.05 was considered statistically significant. Statistical analyses were performed with SPSS software (version 17.0, Chicago, Illinois, USA).
Ethical considerations
The study was approved by the Ethical Committee of the IBD Clinical and Research Centre, ISCARE, Reference Number 2019/IVa.
Results
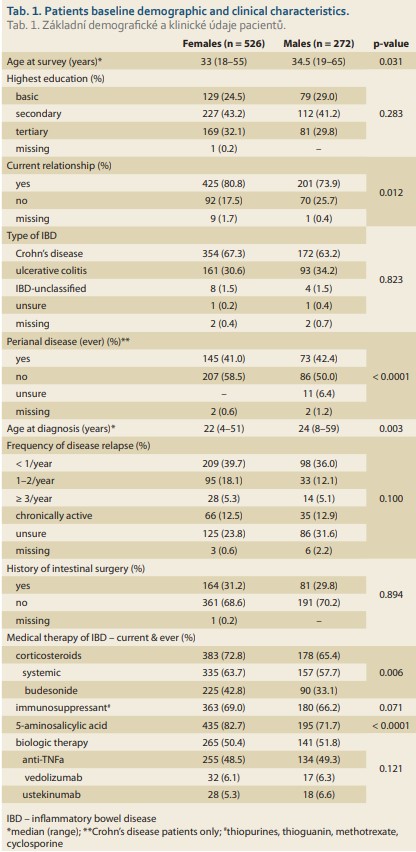
A total of 535 female and 278 male patients with IBD participated in the survey. Of these, 9 (1.7%) females and 6 (2.2%) males were excluded from the analysis due to their age and/or missing information on parenthood. Thus, the final cohort comprised 526 women and 272 men of whom 58.0% and 92.6%, respectively, were recruited during their visit to a gastroenterology centre and the remaining patients participated via an online survey. The baseline demographic and clinical characteristics of the included patients are presented in Tab. 1.
Impact of IBD on reproductive behaviour and plans
There was a significant gender difference in the impact of the disease on reproductive behaviour and plans among patients with IBD (Tab. 2). About one-half of the females (53.2%) and one-fourth of the males (26.8%) indicated at least some limitation in their sexual life due to IBD. Up to 55.5% of the women confessed having a fear of infertility due to IBD and 27.6% reported that the disease influenced (mainly negatively) their earlier reproductive plans with regard to their decision to have no children, to have fewer children, or another timing of pregnancy than previously wished. However, this was the case in only 22.4% and 11.0% of the male patients, respectively (Tab. 2).
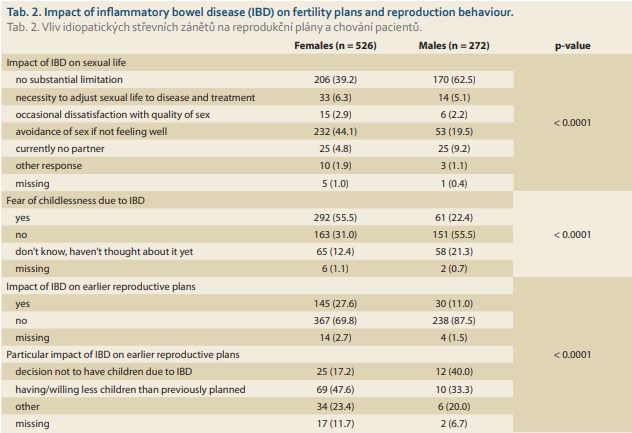
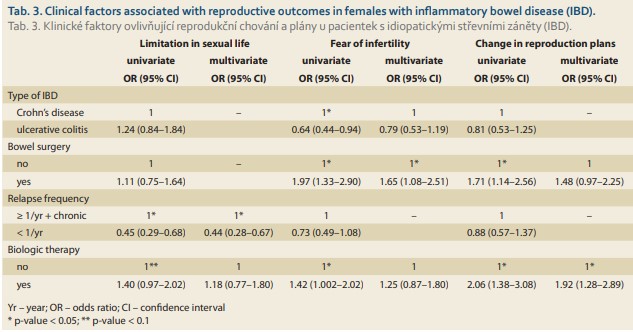
In univariate analyses (Tab. 3), women with higher frequency of relapses or chronic active disease reported significantly more limitations in their sexual lives while females with Crohn’s disease, those with a history of bowel surgery and ever use of biologic therapy were more worried about infertility. The last two factors were also associated with more frequent changes in previous reproductive plans. In the multivariate model, significant factors associated with the outcomes were relapse frequency and limitations in sexual life, history of bowel surgery and fear of infertility and ever use of biologics and change of reproductive plans (Tab. 3).
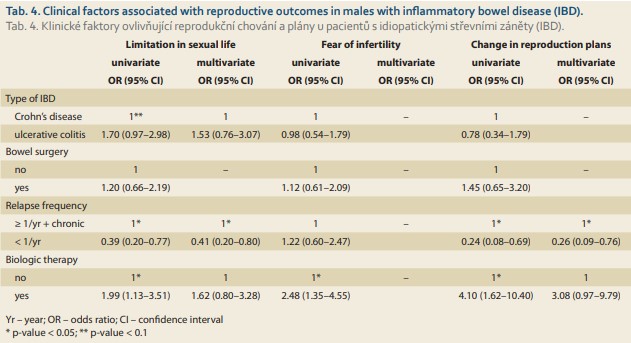
In men, univariate analyses revealed that a higher relapse frequency or chronic active disease and ever use of biologics significantly increased the proportion of patients with limitations in their sexual lives as well as with changes in their previous reproductive plans, while more individuals ever treated with biological therapy reported fears of infertility due to IBD (Tab. 4). In the multivariate model, only relapse frequency remained significantly associated with limitations in sexual life and changes in reproductive plans (Tab. 4).
Parenthood
At the time of survey, 305 (58.0%) females and 128 (47.1%) males already had offspring (median 2 children for both genders; 38.6% and 46.2% of children, respectively, born before the diagnosis of IBD). Most of the patients had their first child born before the age of 30 years (75.4% of women and 60.9% of men) and none after the ages of 40 and 50 years, respectively. Importantly, one-third of the females (102, 33.4%) conceived at least one of their children unintentionally, with 62 females (20.3%) doing so after their diagnosis of IBD. Twenty-two women (7.2%) became pregnant at least once after using assisted reproductive technology (ART) treatment. Among the males, 39 (30.5%) had ≥ 1 of their offspring unintentionally and 5 (3.9%) needed ART therapy.
Childlessness
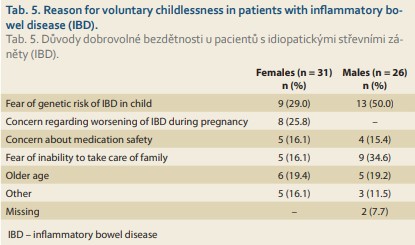
Of the childless patients, 157 (71.0%) women and 100 (69.4%) men were planning to have children in future, 33 (14.9%) and 18 (12.5%) were yet to decide, while 31 (14.0%) females and 26 (18.1%) males were voluntarily childless. Among the voluntarily childless patients, 58.1% of the females and 42.3% of the males confessed that their IBD was the primary cause. The particular reasons for voluntary childlessness are outlined in Tab. 5.
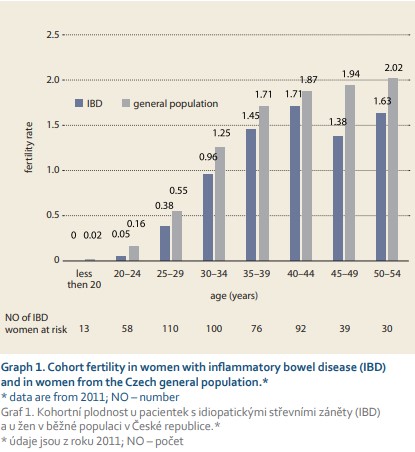
Fertility rate in females
The total fertility rate in women with IBD was lower than in the general population with 1.004 live births per IBD woman versus 1.69 live births per woman in the general Czech population of women in the reproductive age between 15 and 49 years (data available from the year 2017). This pattern of decreased fertility among IBD females was observed in all age-specific categories (Graph 1).
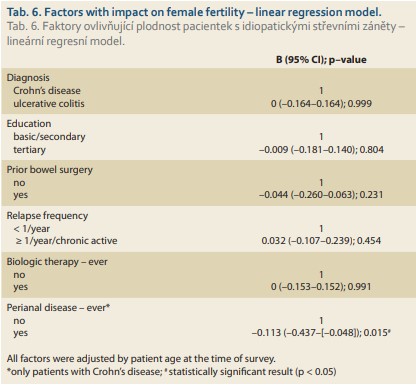
A linear regression model revealed only current or past perianal disease in females with Crohn’s disease to be associated with reduced fertility (ß –0.113; 95%: –0.437 – [–0.048]; p = 0.015). No impact of education, type of IBD, history of previous bowel surgery, ever use of biological therapy or relapse frequency on fertility rate was observed in our study (Tab. 6).
Patient information about IBD reproduction-related issue
Only 320 (60.8%) females and 55 (20.2%) males ever consulted a physician about reproduction-related issues. The majority of them discussed these issues with a gastroenterologist (53.6% of females and 18.4% of males), followed by a gynaecologist/urologist (36.3% / 1.8%) and only a minority approached a general practitioner (3.2% and 1.5%, respectively). Of those consulting a physician, 76.9% of the women and 76.4% of the men were satisfied with the information provided. Regarding the knowledge on medication safety during pregnancy, 20.9% of the females and 15.4% of the males thought that IBD-related medication might have a negative impact when given during pregnancy while 22.4% and 29.4% of them, respectively, were unsure about drug safety. In both genders, the drugs most commonly believed to be harmful were corticosteroids and thiopurines, followed by biological treatment.
Discussion
This is the first study investigating several aspects of reproductive life in patients with IBD in the Czech Republic. The results of the survey demonstrated that the disease had a negative impact on patients’ reproductive behaviour with regard to limitations in sexual life, concerns about potential infertility and changes of attitudes toward childbearing. This negative impact of IBD was expressed significantly more in females. Clinical factors reflecting disease severity were associated with these negative outcomes, both in males and females. The fertility rate in women with IBD from our cohort was lower compared to the background Czech population. Current or past presence of perianal disease in females with Crohn’s disease was associated with decreased fertility. Patient IBD-related reproductive knowledge was inadequate and likely to be at least partially related to insufficient communication between patients and physicians about this issue.
We observed a significantly different impact of IBD on several aspects of reproductive life in males and females despite similar baseline clinical characteristics of both genders. This difference in the perception of fertility issue among patients with IBD was also found in an Australian study where 54% of the female and 32.5% of the male patients experienced fear of infertility (p = 0.035) [7]. Similarly, more females reported a negative impact of IBD on sexual activity than the males (66 % versus 40.5 %; p < 0.0001) [11]. A disease course characterised by a higher frequency of relapses or chronic disease activity, a history of bowel surgery or the need for biological treatment were found to be negatively associated with some reproduction-related outcomes in our cohort. All these factors are related to disease severity, thus patients with a more severe disease are more likely to be negatively influenced by their disease.
Both the total and the cohort fertility rate in female patients from our survey were lower than in the general Czech population. Our results are in agreement with other previous studies showing reduced fertility rates compared to females from background populations [2]. As already mentioned, except for some patient groups (e. g. history of small pelvis surgery, active disease), fertility in patients with IBD is considered to be similar to the general population [3,4,12–14]. Indeed, 7% of our IBD women needed ART treatment to conceive at least one of their children, which roughly corresponds to population data with about 4% of all children born alive in the Czech Republic in 2017 after ART treatment [15,16]. However, a higher rate of voluntary infertility has been described, mainly in females, than in healthy individuals [2]. According to a French systematic review, voluntary childlessness in females with IBD ranged between 14% and 36% [2]. In our cohort, 14% of childless women and 18% of childless men (6% and 10% of all study female and male population, respectively) were voluntarily childless. Unfortunately, corresponding figures for the general Czech population are missing. The most frequent reason for voluntary childlessness in our patients was concern regarding the heritability of IBD, followed by fear of the disease worsening during pregnancy in females and worries about their inability to take care of their families in males. These findings are in line with previous literature evidence [5–7]. Of note, a considerable proportion of our females (13% of all women studied) changed their earlier reproductive plans and decided to have fewer children than previously wished. A similar attitude was observed also in an Australian study where approximately one-fourth of IBD patients with children reported having fewer children than they desired [7]. The current or past presence of perianal disease in our females with Crohn’s disease was negatively associated with fertility. Perianal disease is a predictor of a poor long--term outcome of IBD and has a significantly negative impact on the patient’s quality of life [17]. Further, the presence of fistulising Crohn’s disease may contribute to sexual dysfunction and thus have an indirect negative effect on reproductive behaviour [18].
Up to 20% of our females with an already established diagnosis of IBD conceived at least one of their children unplanned. This is in discrepancy with the general recommendation that women with IBD should always plan their pregnancies for the remission period to minimise the risk of flare-up during pregnancy, potential pregnancy complications and adverse pregnancy outcomes [3,4]. Furthermore, over 40% of our patients had either inadequate or insufficient awareness about medication safety during pregnancy. This might be partially related to the fact that only around 60% of our females and 20% of our males ever discussed reproduction-related issues with their physician. The low rate of consultation between patients and physicians regarding this issue has also been described in previous studies and was very likely the cause of poor IBD-related reproductive knowledge and misperceptions found in a considerable proportion of the patients [5,8,9].
The strength of our study is that this is the first study investigating IBD-specific reproductive issues from the patients’ perspective in the Czech Republic and to our knowledge, also in Central and Eastern Europe. Currently, there is no validated questionnaire to study this topic. Therefore, we tried to increase the comprehensibility and relevance of the questionnaire for patients by collaboration with Patient Organisation, both in the process of creation of the questionnaire and in the testing of the final version in a small group of patients prior to start of the survey.
Our study has several limitations which have to be acknowledged. Firstly, the study cohort represents a population with more severe disease, as about one-half of the individuals received biological therapy. It is estimated that approximately 20% of the Czech patients with Crohn’s disease and 10% with ulcerative colitis were ever exposed to biological therapy. Thus, the anticipated higher rate of more severe cases of IBD included in our survey might have had an impact on our findings. Secondly, although the sample size compared to already published studies was relatively high, it was still limited, mainly in the male cohort and for the calculation of cohort fertility. This fact, together with the relatively young age of the study population might have had an influence on our finding of a lower fertility rate in females with IBD compared to the general population. Further, more recent data on cohort fertility in females (last data available from 2011) and data on male fertility in the Czech background population are lacking. Finally, information on the disease course and medication was patient-reported with a potential risk of imprecision and recall bias.
In conclusion, our study demonstrated that IBD has a negative impact on several aspects of patients’ reproductive behaviour. This impact was especially obvious in females and individuals with a more severe disease course. The fertility rate in women with IBD in our survey was lower than in the general population, and the negative impact of IBD seemed to contribute most to these findings. Better communication between patients and physicians is necessary to improve these unfavourable outcomes.
Acknowledgements
The authors wish to thank all participating centres which included patients in the study.
Submitted/Doručeno: 5. 11. 2020
Accepted/Přijato: 20. 11. 2020
Dana Ďuricová, MD, PhD.
Clinical and Research Centre for IBD ISCARE a.s.
Českomoravská 2510/19
190 00 Praha 9
Czech Republic
dana.duricova@seznam.cz
To read this article in full, please register for free on this website.
Benefits for subscribers
Benefits for logged users
Literature
1. Duricova D, Burisch J, Jess T et al. Age-related differences in presentation and course of inflammatory bowel disease: an update on the population-based literature. J Crohns Colitis 2014; 8 (11): 1351–1361. doi: 10.1016/j.crohns.2014.05.006.
2. Tavernier N, Fumery M, Peyrin-Biroulet L et al. Systematic review: fertility in non-surgically treated inflammatory bowel disease. Aliment Pharmacol Ther 2013; 38 (8): 847–853. doi: 10.1111/apt.12478.
3. Mahadevan U, Robinson C, Bernasko N et al. Inflammatory bowel disease in pregnancy clinical care pathway: a report from the american gastroenterological association IBD parenthood project working group. Gastroenterology 2019; 156 (5): 1508–1524. doi: 10.1053/j.gastro.2018.12.022.
4. van der Woude CJ, Ardizzone S, Bengtson MB et al. The second European evidenced-based consensus on reproduction and pregnancy in inflammatory bowel disease. J Crohns Colitis 2015; 9 (2): 107–124. doi: 10.1093/ecco-jcc/jju006.
5. Marri SR, Ahn C, Buchman AL. Voluntary childlessness is increased in women with inflammatory bowel disease. Inflamm Bowel Dis 2007; 13 (5): 591–599. doi: 10.1002/ibd.20082.
6. Ellul P, Zammita SC, Katsanos KH et al. Perception of reproductive health in women with inflammatory bowel disease. J Crohns Colitis 2016; 10 (8): 886–891. doi: 10.1093/ecco-jcc/jjw011.
7. Mountifield R, Bampton P, Prosser R et al. Fear and fertility in inflammatory bowel disease: a mismatch of perception and reality affects family planning decisions. Inflamm Bowel Dis 2009; 15 (5): 720–725. doi: 10.1002/ibd.20839.
8. Mountifield R, Andrews JM, Bampton P. It IS worth the effort: patient knowledge of reproductive aspects of inflammatory bowel disease improves dramatically after a single group education session. J Crohns Colitis 2014; 8 (8): 796–801. doi: 10.1016/j.crohns.2013.12.019.
9. Selinger CP, Eaden J, Selby W et al. Inflammatory bowel disease and pregnancy: lack of knowledge is associated with negative views. J Crohns Colitis 2013; 7 (6): e206–e213. doi: 10.1016/j.crohns.2012.09.010.
10. Český statistický úřad. Plodnost žen. Praha 2013 [online]. Dostupné na: https: //www.czso.cz/documents/10180/20551769/170224-14.pdf/287dc43c-df94-40c1-bf04-b322ed0e4b84?version=1.0.
11. Muller KR, Prosser R, Bampton P et al. Female gender and surgery impair relationships, body image, and sexuality in inflammatory bowel disease: patient perceptions. Inflamm Bowel Dis 2010; 16 (4): 657–663. doi: 10.1002/ibd.21090.
12. Rajaratnam SG, Eglinton TW, Hider P et al. Impact of ileal pouch-anal anastomosis on female fertility: meta-analysis and systematic review. Int J Colorectal Dis 2011; 26 (11): 1365–1374. doi: 10.1007/s00384-011-1274-9.
13. Ban L, Tata LJ, Humes DJ et al. Decreased fertility rates in 9639 women diagnosed with inflammatory bowel disease: a United Kingdom population-based cohort study. Aliment Pharmacol Ther 2015; 42 (7): 855–866. doi: 10.1111/apt.13354.
14. Ananthakrishnan AN, Martin C, Kane S et al. Paternal disease activity is associated with difficulty in conception among men with inflammatory bowel diseases. Clin Gastroenterol Hepatol 2019; 17 (1): 203–204. doi: 10.1016/j.cgh.2018.04.001.
15. Český statistický úřad. Demografická příručka. Praha 2017 [online]. Dostupné na: https: //www.czso.cz/csu/czso/demograficka-prirucka-2017.
16. Ústav zdravotnických informací a statistiky ČR. Asistovaná reprodukce v ČR 2017. Praha 2019 [online]. Dostupné na: https: //www.uzis.cz/res/f/008274/asistreprodukce2017.pdf.
17. Panés J, Rimola J. Perianal fistulizing Crohn’s disease: pathogenesis, diagnosis and therapy. Nat Rev Gastroenterol Hepatol 2017; 14 (11): 652–664. doi: 10.1038/nrgastro.2017.104.
18. Martin J, Kane SV, Feagins LA. Fertility and contraception in women with inflammatory bowel disease. Gastroenterol Hepatol (NY) 2016; 12 (2): 101–109.