Assessment of home biofeedback training efficacy in fecal incontinence using anal sphincter pressure response to cough reflex
Marek Vojtko1, Peter Lipták1, Branislav Malý1, Peter Bánovčin1
+ Affiliation
Summary
Background: Fecal incontinence is defined as the recurrent uncontrolled passage of feces. It is a relatively common disorder with a prevalence of up to 7% of the population worldwide. The therapy for fecal incontinence should be individualized, such as biofeedback training. However, there is no universal consensus on the method of evaluating its efficacy. Aim and methods: To evaluate the utility of the cough maneuver for assessing the efficacy of anal sphincter training. This is a retrospective analysis of a cohort of patients with fecal incontinence who underwent home biofeedback training with local electric stimulation for 3 months. Results: During the analyzed period, 50 patients were randomly assigned to one of two types of devices based on current availability. Data from 29 patients have been evaluated for the final analysis. Statistically significant improvements were found in rest maximum pressure, voluntary maximum pressure, and Wexner score when comparing the pre- and post-intervention. However, differences in rest mean pressure and pressure during cough were not significant, although there was a tendency toward post-intervention improvement. Conclusion: The data presented here provide evidence that home-based biofeedback training with local stimulation presents an effective alternative to office-based biofeedback training in patients with fecal incontinence. Besides the standard manometry parameters utilized for anorectal function assessment, the pressure during voluntary cough could provide a clinical utility even in patients without spine or peripheral nerve lesions, but further studies are needed to evaluate this hypothesis.
Keywords
fecal incontinence, manometry, home biofeedback, stimulation, cough
Introduction
Fecal incontinence (FI) is defined as recurrent uncontrolled passage of fecal material for at least 3 months [1]. FI is relatively common, with a prevalence of up to 7% of the population worldwide [2] , and it is higher in women [3] than in men. Therapy for fecal incontinence should be individualized based on symptom presentation [4]. Biofeedback training (BFB) is a highly personalized method of therapy, and it is administered when there is a possibility that the patient could learn voluntary control of the response to the disease presentation. It involves practicing and improving motor skills using extended feedback on physiological signals to a gradually increasing physiological stimulus with the aim of improving its perception [5]. It is recommended by the joint position of the American Neurogastroenterology and Motility Society (ANMS) and the European Society of Neurogastroenterology and Motility (ESNM) for short and long-term treatment of fecal incontinence in adults [6]. However, the availability of biofeedback training is not universal, and it‘s mostly performed in specialized centers. Furthermore, it is significantly time-consuming, and it substantially raises the cost of medical care. Home-administered biofeedback presents an emerging time- and cost-saving alternative to the office setting. However, there are only scarce published data analyzing this novel approach [7– 9]. Moreover, there is no universal consensus on the method of evaluating its efficacy in fecal incontinence. The standard method to objectively asses the anorectal function is anorectal manometry [10]. Among various parameters used in the assessment of anorectal function according to the IAPWG [11] protocol, the cough reflex test represents a clinically relevant, non-invasive method to evaluate reflexive contraction of the external anal sphincter (EAS) and associated pelvic floor muscles. During a cough, increased intra-abdominal pressure activates a coordinated neuromuscular response in order to stop involuntary leakage of stool or gas. This polysynaptic reflex mediates both somatic and autonomic responses. It is not present or weak in patients with serious spine or peripheral nerve injury. Although included in the IAPWG protocol as one of the steps in anorectal function examination, the evaluation is not reflected by the London consensus criteria [11]. The clinical relevance of examining this reflex in patients without known or significant spine injury is unknown. Therefore, we decided to retrospectively analyze data from patients who underwent home biofeedback therapy for fecal incontinence and compare pre- and post-intervention manometry values during the cough reflex to establish a first step for further investigation and assessment of the utility of this reflex in broader settings.
Methods
This is a retrospective analysis of a patient cohort with a diagnosis of fecal incontinence who received home biofeedback with local electrical stimulation as a therapeutic method. Two different commercially available devices were used with two different training and stimulation programs. Modality one utilized frequency: 40 Hz; Impulse width: 0.2 s; Ramp up time: 1 s; Work out time: 6 s; Rest: 15 s; and Training duration: 20 min. The second modality utilized continual stimulation with 35 Hz, 0.33 Impulse width, followed by workout: Frequency: 30 Hz; Impulse width: 0.25 s; Ramp up time: 0.3 s; Work out time: 5 s; Ramp down time: 0.3 s; and Rest 5 s. Training duration: 6 + 20 min.
Duration of therapy was 3 months. On the first visit, 3D HD anorectal manometry was used according to the shortened IAPWG protocol (measurement of rest pressure, 4-times voluntary contraction, cough). Wexner‘s self-reporting questionnaire was provided to the patients in order to measure not only the objective manometry data, but also to evaluate the subjective clinical presentation of symptoms. After the measurement, patients were randomly provided with therapeutic devices for home training. An extensive consultation and explanation of the method and procedure was provided by the attending clinician. A contact for troubleshooting consultation was provided. Patients were instructed to train 6 times a week, one time daily. A warning not to use the local current higher than 25mA was provided both verbally and in written form to avoid possible adverse events. After 3 months, at the follow-up visit, the repeated 3D HD anorectal manometry and Wexner score were evaluated.
Data acquisition and storage were done by Excel (Microsoft, USA). Excel performed the statistical analysis and assistance with statistical interpretation was provided by OpenAI (San Francisco, CA).
The effect of the intervention was evaluated using both the paired t-test and Wilcoxon signed-rank test. The assumption of normality of the paired differences was tested using the Shapiro-Wilk test. As the distribution of differences was non-normal, the non-parametric Wilcoxon test was preferred for inferential analysis. Statistical significance was defined as P < 0.05. Additionally, the effect size was calculated using Cohen’s D, with values interpreted according to conventional thresh- olds (0.2 = small, 0.5 = moderate, and 0.8 = large).
The evaluated manometry parameters were rest mean pressure, rest maximum pressure, maximum voluntary pressure, and maximum pressure during voluntary cough. Figures were drawn in Plotly (plotly.com).
Results
During the analyzed period (9/ 2022– 4/ 2025), 50 patients were randomly assigned modality one or modality two based on current availability. From the total, 21 patients did not attend the control visit, refused the repeated anorectal manometry, or the cough reflex was not adequately evaluated during the procedure. These patients were excluded from the analysis. Therefore, data from 29 patients were evaluated for the final analysis. From this total, 26 were female and two were male. The average age was 57.9 years. In 19 patients, modality 1 was used, and in 9 patients, modality 2 was used. The specific parameters were evaluated as follows:
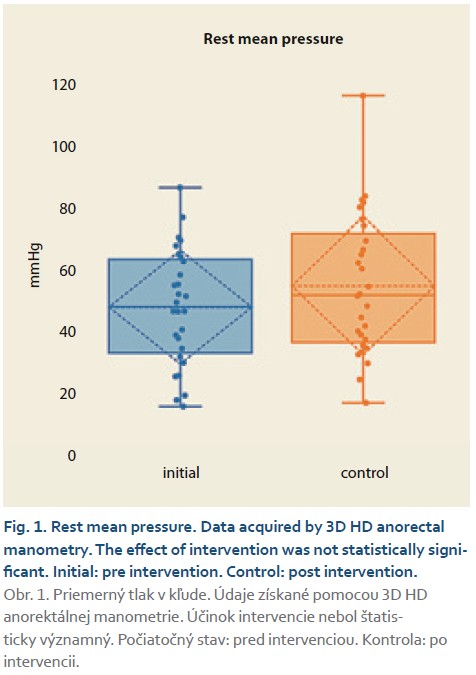
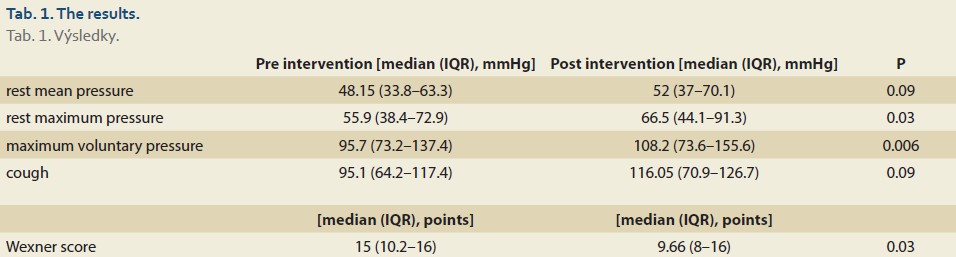
- Rest mean pressure (Fig. 1): No significant differences were found comparing the pre- and post-intervention pressure values (P = 0.089) with a small to moderate effect calculated as Cohen’s D (0.32).
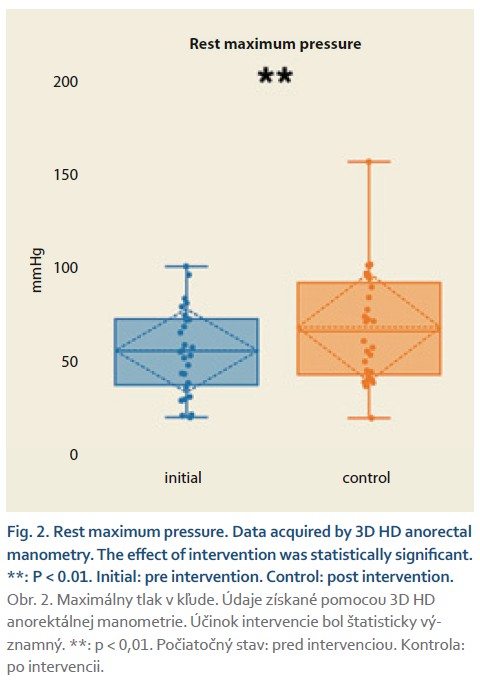
- Rest maximum pressure (Fig. 2): Statistically significant differences were found comparing the pre- and post-intervention pressure values (P < 0.01) with a medium effect calculated as Cohen’s D (0.41).
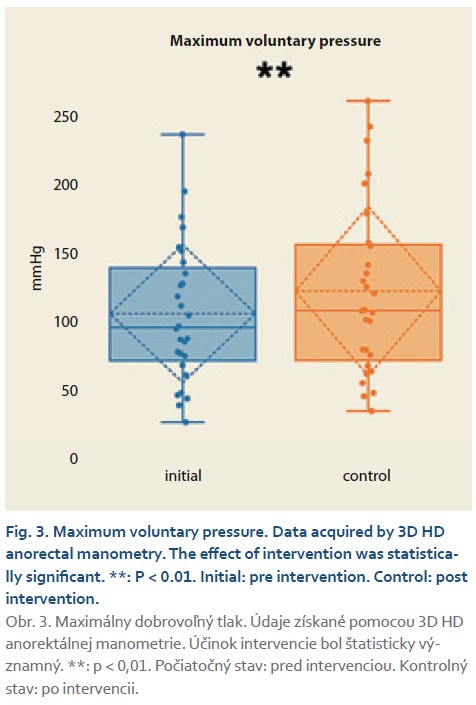
- Voluntary maximum pressure (Fig. 3): Statistically significant differences were found comparing the pre- and post-intervention pressure values (P < 0.01) with a medium effect calculated as Cohen’s D (0.57).
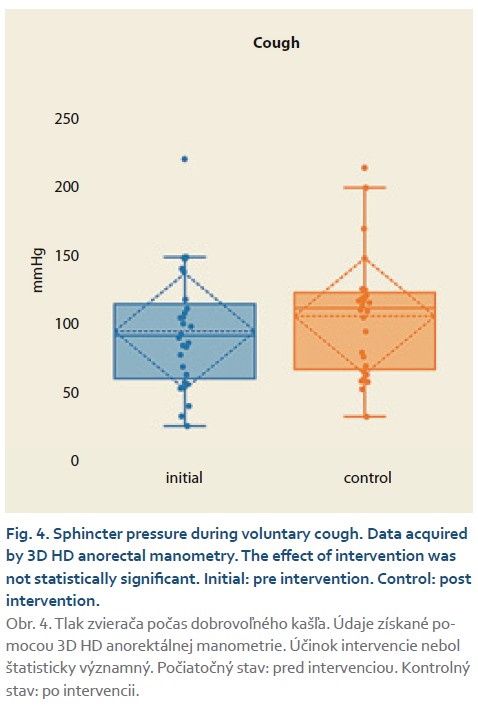
- Cough pressure (Fig. 4): No statistically significant differences were found comparing the pre- and post-intervention pressure values (P = 0.09) with a small to moderate effect calculated as Cohen’s D (0.35).
- Wexner score: Statistically significant differences were found comparing the pre- and post-intervention pressure values (P < 0.5) with a medium effect calculated as Cohen’s D (0.53).
The results are further summarized in Tab. 1.
Discussion
Joined effort by the United European Gastroenterology (UEG), European Society of Neurogastroenterology and Motility (ESNM), European Society of Coloproctology (ESCP), and European Society of Primary Care Gastroenterology (ESPCG) resulting in the European guidelines for the diagnosis and treatment of fecal incontinence, consider biofeedback therapy as one of the first-line treatment options [12]. On the other hand, the effect of home biofeedback has not been evaluated. Furthermore, biofeedback should be considered for patients with failed conservative treatment, and where there is no option available in terms of more invasive procedures [13]. A crucial factor is the ability to comply with the treatment protocol [14] , as this is the main factor for introducing long-term sustainability of anorectal function [15]. However, there is no universally adopted protocol for home or office-based biofeedback [16]. Several studies are focusing on the development of an appropriate protocol for home biofeedback training [17]. After initial utility and compliance testing, our center adopted the protocol in which the length of therapy is 3 months, with training performed once daily, six times a week. This is further used in our clinical practice. Our results show that adhering to this protocol leads to a significant improvement in the rest maximum pressure and voluntary squeeze pressure in the analyzed cohort. This is in agreement with the results of the randomized control study by Bartlett et al. [18]. The same is true when comparing subjective symptom reporting. Our data point to the significant improvement of the Wexner score. Interestingly, while Bartlett focused on young patients, the average age in our cohort was 58 years. This indicates that age is probably not the main factor influencing the efficacy of BFB. The second published randomized controlled study regarding home biofeedback was performed by Xiang et al. [9]. This group also reported the positive effect of home biofeedback on symptoms and objective anorectal function in patients with FI. Furthermore, they concluded that it is not inferior to office-based biofeedback. The above-mentioned studies support our finding of home biofeedback efficacy, even utilizing different protocols and therapy devices. Previously published data from different study groups showed that even electric stimulation alone could provide improvement of anorectal function in patients with fecal incontinence [19,20]. To the best of our knowledge, there are no published data so far evaluating the effect of the combination of voluntary anorectal muscle training and electrical stimulation. However, as the presented data are a combination of two different types of devices with different training protocols, the primary aim of this study is not to evaluate the efficacy of home biofeedback with stimulation per se, but to investigate the possible role of the cough reflex maneuver in the efficacy evaluation of anorectal training. The need for more objective parameters to be assessed results from the outcomes of studies that suggested that the placebo effect could also play an important role in influencing the patient efficacy perception [21]. Based on the physiological non-voluntary nature of the cough reflex, it is possible to argue that it could present a valid assessment parameter complementing rest pressure assessment and maximum voluntary squeeze assessment. Especially the latter is primarily influenced by the voluntary control of the patient, which could be further influenced by various personal aspects.
The cough-induced contraction of the anal sphincter is involuntary and its effect depends on the reflex arc integrity. This reflex consists of sensorimotor pathways, neuromuscular communications, and muscle responses. Specifically, the reflex is initiated by afferent signals originating from mechanoreceptors in the thoracic cavity and are conducted via the vagal nerve. Then, they are integrated in the brainstem and in spinal segments. As the efferent component is activated, it involves the action of the pudendal nerve that innervates the striated muscles of the external anal sphincter. This leads to rapid contraction of these muscles and prohibits the leakage of stool during increased abdominal pressure during coughing. As biofeedback training is effective mainly in the striated muscles, we hypothesized that the pressure measured by anorectal manometry during coughing could be influenced by the training. Although our results showed that indeed the average sphincter pressure in our cohort during the cough is higher post-intervention compared to pre-intervention, this difference is not significant and has a low clinical effect. This implies that evaluating the cough reflex as an objective measurement of intervention could have its clinical implication; however, further studies are needed to assess this hypothesis.
Limitations of this study lie in its retrospective character, heterogeneous population, and type of intervention. On the other hand, data published so far regarding this topic are scarce and thus our results could present a base for further, more rigorous investigation such as randomized controlled trials which will take into consideration different incontinence phenotypes, sexes, and/ or interventions. The cough reflex could become a focus of these studies to confidently assess its possible utilization and diagnostic value in fecal incontinence in patients without spine injury.
Conclusion
Here the presented data provide evidence that home-based training presents an effective alternative to office--based training in patients with fecal incontinence. Beside the standard manometry parameters utilized for anorectal function assessment, the pressure during a voluntary cough could provide a clinical benefit even in patients without spine or peripheral nerve lesions, but further studies are needed to evaluate this hypothesis.
ORCID authors
P. Lipták 0000-0001-8257-8567,
B. Malý 0009-0005-9280-8377,
P. Bánovčin 0000-0001-6694-9364.
Submitted/ Doručené: 27. 6. 2025
Accepted/ Prijaté: 8. 8. 2025
Corresponding author
Peter Lipták, MD, PhD
Clinic of Internal Medicine – Gastroenterology
Jessenius Faculty of Medicine in Martin, Comenius University
University Hospital in Martin
Kollarova 2
03601 Martin
peter.liptak@uniba.sk
To read this article in full, please register for free on this website.
Benefits for subscribers
Benefits for logged users
Literature
1. Rao SS, Bharucha AE, Chiarioni G et al. Anorectal disorders. Gastroenterology 2016; 150(6): 1430.e4– 1442.e4.
2. Bharucha AE, Knowles CH, Mack I et al. Faecal incontinence in adults. Nat Rec Dis Primers 2022; 8(1): 53. doi: 10.1038/ s41572-022-00381-7.
3. Landefeld CS, Bowers BJ, Feld AD et al. National Institutes of Health state-of-the-science conference statement: prevention of fecal and urinary incontinence in adults. Ann Intern Med 2008; 148(6): 449– 458. doi: 10.7326/ 0003-4819-148-6-200803180-00210.
4. Menees S, Chey WD. Fecal incontinence: pathogenesis, diagnosis, and updated treatment strategies. Gastroenterol Clin North Am 2022; 51(1): 71– 91. doi: 10.1016/ j. gtc.2021.10.005.
5. Chiarioni G, Whitehead WE. The role of biofeedback in the treatment of gastrointestinal disorders. Nat Clin Pract Gastroenterol Hepatol 2008; 5(7): 371– 382. doi: 10.1038/ ncpgasthep1150.
6. Rao SS, Benninga MA, Bharucha AE et al. ANMS-ESNM position paper and consensus guidelines on biofeedback therapy for anorectal disorders. Neurogastroenterol Motil 2015; 27(5): 594– 609. doi: 10.1111/ nmo.12520.
7. Xiang X, Sharma A, Patcharatrakul T et al. Is home biofeedback training useful for fecal incontinence: preliminary results of RCT with new home device. Am J Gastroenterol 2017; 112: S254. doi: 10.14309/ 00000434-201710001-00481.
8. Sharma A, Xiang X, Yan Y et al. Home biofeedback therapy improves fecal incontinence severity and quality of life in a non-inferiority randomized controlled study. Am J Gastroenterol 2018; 113: S246. doi: 10.14309/ 00000434-201810001-00416.
9. Xiang X, Sharma A, Patcharatrakul T et al. Randomized controlled trial of home biofeedback therapy versus office biofeedback therapy for fecal incontinence. Neurogastroenterol Motil 2021; 33(11): e14168. doi: 10.1111/ nmo.14168.
10. Belilos EA, Post Z. Anderson S et al. The clinical utility of anorectal manometry: a review of current practices. Gastro Hep Adv 2025; 4(2): 100562. doi: 10.1016/ j. gastha.2024.10.002.
11. Carrington EV, Heinrich H, Knowles CH et al. The international anorectal physiology working group (IAPWG) recommendations: standardized testing protocol and the London classification for disorders of anorectal function. Neurogastroenterol Motil 2020; 32(1): e13679. doi: 10.1111/ nmo.13679.
12. Assmann SL, Keszthelyi D, Kleijnen J et al. Guideline for the diagnosis and treatment of faecal incontinence – A UEG/ ESCP/ ESNM/ ESPCG collaboration. United European Gastroenterol J 2022; 10(3): 251– 286. doi: 10.1002/ ueg2.12213.
13. Norton C. Fecal incontinence and biofeedback therapy. Gastroenterol Clin North Am 2008; 37(3): 587– 604. doi: 10.1016/ j. gtc.2008.06.008.
14. Bartlett L, Sloots K, Nowak M et al. Biofeedback therapy for faecal incontinence: a rural and regional perspective. Rural Remote Health 2011; 11(2): 1630.
15. Ozturk R, Niazi S, Stessman M et al. Long-term outcome and objective changes of anorectal function after biofeedback therapy for faecal incontinence. Aliment Pharmacol Ther 2004; 20(6): 667– 674. doi: 10.1111/ j. 1365-2036.2004.02125.x.
16. Vasant DH, Solanki K, Balakrishnan S et al. Integrated low-intensity biofeedback therapy in fecal incontinence: evidence that “good” in-home anal sphincter exercise practice makes perfect. Neurogastroenterol Motil 2017; 29(1): e12912. doi: 10.1111/ nmo.12912.
17. Rao SS. Keys to the diagnosis and management of patients with fecal incontinence. Gastroenterol Hepatol (N Y) 2022; 18(3): 169– 171.
18. Bartlett L, Sloots K, Nowak M et al. Supplementary home biofeedback improves quality of life in younger patients with fecal incontinence. J Clin Gastroenterol 2015; 49(5): 419– 428. doi: 10.1097/ MCG.0000000000000143.
19. Berghmans B, Bols E, Seleme M et al. Behavioral therapies and biofeedback for anal incontinence. In: Pelvic floor disorders. Springer 2021: 459– 472.
20. Cohen-Zubary N, Gingold-Belfer R, Lambort I et al. Home electrical stimulation for women with fecal incontinence: a preliminary randomized controlled trial. Int J Colorectal Dis 2015; 30(4): 521– 528. doi: 10.1007/ s00384-015-2128-7.
21. Enck P, Van der Voort IR, Klosterhalfen S. Biofeedback therapy in fecal incontinence and constipation. Neurogastroenterol Motil 2009; 21(11): 1133– 1141. doi: 10.1111/ j. 1365-2982.2009. 01345.x.