Epidemiological and demographic characteristics of individuals with irritable bowel syndrome based on the Rome III vs. Rome IV criteria in the Northern part of Serbia
Dusan Slankamenac1, Darko Dabic2, Aleksandra Dabic3, Tamara Slankamenac4, Andrej Preveden4,5
+ Affiliation
Summary
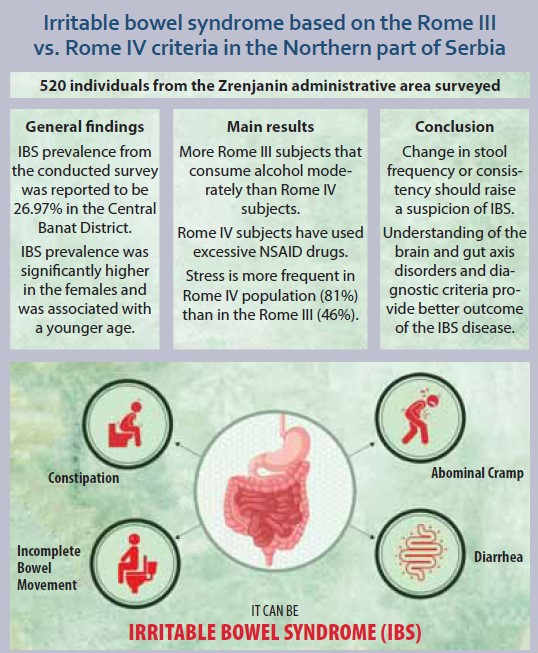
Background: Rome IV diagnostic criteria offer a new definition of IBS as opposed to Rome III. Practically, there have been 3 main changes made from the Rome III criteria to IV, such as abdominal discomfort, the threshold for the frequency of abdominal pain, and the relation of abdominal pain in IBS to defecation. The aims of this study were epidemiology of the IBS population and comparison of the characteristics of the subjects who fulfill Rome III vs. those who fulfill both III and IV criteria with regard to the IBS diagnosis. Methods: A sample of adult healthy population from the Municipality of Zrenjanin area was investigated through a questionnaire. All the subjects were approached from 5th March to 17th June, 2020. The study was submitted to and approved by the local Ethics Committee at the city hospital. Results: Based on the conducted survey in the Zrenjanin area, the IBS prevalence was reported to be 26.97% based on Rome III criteria. A larger number of women aged 18–21 was reported to have IBS. The most prevalent subtype noted was IBS-C. A significant correlation was noted between smoking, alcohol, drug abuse, other comorbidities, patient characteristics and stress factors in the IBS identified subjects. Conclusions: To sum up, our study recommends young people to be screened for IBS. Any symptom of change in stool frequency or consistency should raise a suspicion of IBS after undergoing all the relevant investigations for ruling out organic diseases. This will aid their early diagnosis and will help to improve their quality of life.
Keywords
irritable bowel syndrome, Rome III criteria, Rome IV criteria, epidemiology
Introduction
Irritable bowel syndrome (IBS) is a functional intestinal disorder characterized by abdominal pain associated with altered bowel habits [1]. Irritable bowel syndrome (IBS) is the most common reason to visit a gastroenterologist. IBS was believed to be a functional disease, but many possible pathophysiologic mechanisms can now explain the symptoms. Notably, irritable bowel syndrome negatively affects the quality of life, which is reflected in reduced productivity in work, as well as more frequent use of health care.
Since the definition of IBS was changed in the Rome IV criteria, differences in diagnosis have been noted. However, it has been challenging to make agreement between the Rome III and IV criteria or the differences between Rome IV-positive and -negative IBS patients. The potential influences of each change on the diagnosis of IBS are also unknown. Is Rome IV IBS the same disease as Rome III IBS with more serious symptoms, or is it a disease that completely differs from Rome III IBS? Answers to these questions are important for evaluating the validity of the criteria and understanding IBS. For the past ten years, the Rome III criteria have been considered as the standard for IBS diagnosis. However, with increasing knowledge of IBS, clinicians have focused more on abdominal pain and altered stool habits when diagnosing IBS. Furthermore, the frequency of abdominal symptoms was re-investigated in IBS patients, and according to dissatisfaction with the existing criteria, the guidelines for symptom frequency in IBS diagnosis were reconfigured [2,3]. As a result, the Rome IV diagnostic criteria offer a new definition of IBS. Practically, there were 3 main changes made from the Rome III criteria to Rome IV. First, abdominal discomfort was removed from the definition of IBS, because this was believed to be an ambiguous term with no equivalent in some languages. It was also hypothesized that regardless of whether the term abdominal pain or abdominal discomfort was used, the same individuals would meet criteria for IBS. Second, the threshold for the frequency of abdominal pain required to meet criteria for IBS was increased from 3 days per month to 1 day per week, which was based on a survey of the frequency of the occurrence of abdominal pain in the general population. Finally, there was an appreciation that abdominal pain in IBS is related to, rather than just relieved by, defecation (Tab. 1) [4].
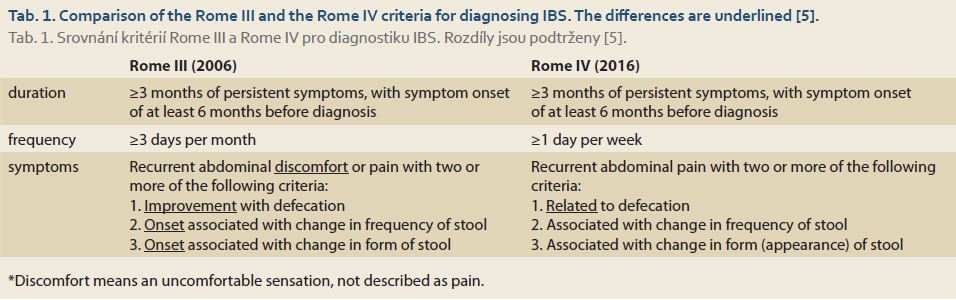
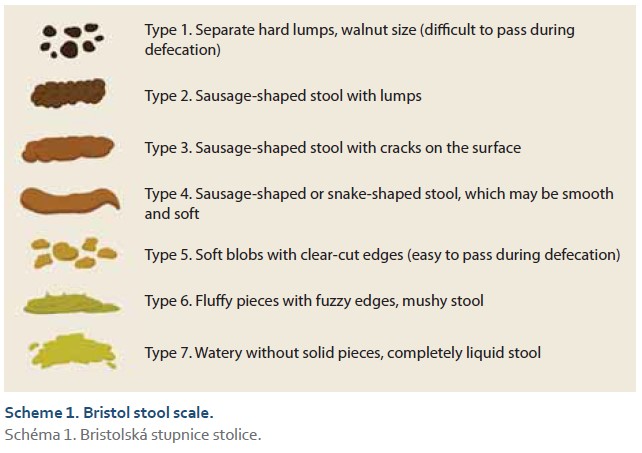
In both definitions, the changes in frequency as in Rome III and or form i.e. appearance of stool is important. Therefore, the Bristol stool scale is a diagnostic medical tool designed to classify the form of human feces into seven categories. It is used in both clinical and experimental fields (Scheme 1).
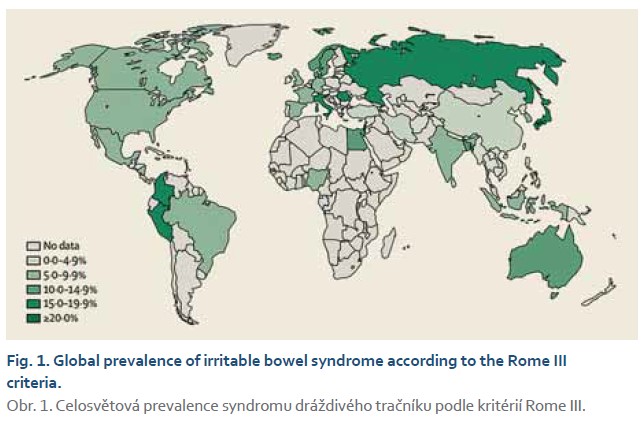
IBS is a prevalent disorder world-wide, with prevalence rates of 5–15% in the Western population [6,7]. Symptoms most likely result from complex interactions between several biological, psychological, and social factors [8,9]. To this date, no specific biomarkers are available to accurately diagnose IBS. Therefore, due to symptom overlap with other bowel diseases, IBS diagnoses are difficult [10].
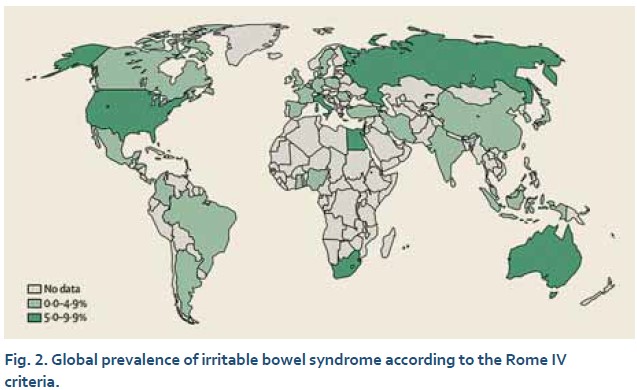
In the one of most recent meta-analysis the lowest prevalence reported was 0.2% in a study from India that used the Rome IV criteria. The highest prevalence was 29.2%, reported in a study from Croatia that used the Rome III criteria. Please see epidemiology data on worldwide depicted on the figures below (Fig. 1, 2) [11].
Since the pathogenesis of IBS is still poorly understood, the question arises whether the intake of medication can contribute to or trigger onset of symptoms in IBS patients, as these patients often utilize medications that may potentially alter intestinal homeostasis. One postulated hypothesis points to increased intestinal permeability in IBS patients induced by exposure to certain medication, such as non-steroidal anti-inflammatory drugs (NSAIDs), thereby allowing luminal antigens to enter the lamina propria and eliciting an immune and inflammatory reaction [12].
The aims of the present study are to identify and publish the epidemiology of the IBS population in the Central Banat District, particularly in the Municipality of Zrenjanin due to the fact that there is little public epidemiology information on the IBS population in this region available. Furthermore, we have compared characteristics of the subjects who fulfill Rome III but do not fulfill the Rome IV vs. those who fulfill the Rome III and Rome IV criteria with a regard to the IBS diagnosis. Also, we have investigated the agreement between the Rome III and Rome IV criteria to identify the differences between Rome IV-positive and -negative IBS patients among the Rome III subjects.
Methods
Participants and setting
The survey was administered randomly to the subjects by trained persons, who received prior training about this study before using the face-to-face interview technique. The subjects were investigated from the Municipality of Zrenjanin urban and local rural settlements. Zrenjanin is a city and the administrative center of the Central Banat District in the Autonomous Province of Vojvodina, Serbia. Based on 2016 census data, the city administrative area has 118,699 inhabitants, which is 1.69% of the total Serbian population. Notably, we have investigated nearly 520 individuals, which is 0.44% of the Zrenjanin administrative area population.
All the subjects older than 18 were approached from 5th March to 17th June, 2020. There were no exclusion criteria.
The study survey and aims of investigation were submitted to and approved by the local Ethics Committee. All the participants were provided with a form of written informed consent to sign, which all of them have signed and ICH guidelines were followed respectively.
Data collection
The survey was divided into 3 sections. The first section covered demographic information such as sex, age, residence, marital status and education, life habits, height and weight, out of which body mass index (BMI) was calculated, as well as dietary habits and general health condition. The second and the third section investigate the Rome III and Rome IV related question, respectively.
Statistical analysis
We calculated the proportions of individuals who self-identified as having IBS who met either the Rome III or the Rome IV criteria for IBS. We measured the agreement between the Rome III and the Rome IV criteria for the presence of IBS by using the modified kappa statistic, where a value <0.2 indicates poor agreement and a value >0.8 indicates excellent agreement beyond chance. A descriptive analysis was performed on all studied variables. The mean ± standard deviation (SD) was used for quantitative variables and the frequencies were used for qualitative variables.
The differences between two groups were assessed by Student’s t-test or the chi-square test. The differences among three groups were assessed by the chi-square test. In this study, the differences with a P-value <0.05 were considered statistically significant. All statistical analyses were performed by using SPSS for Windows version 24.0 (SPSS Inc, Chicago, IL).
Results
Participant characteristics
As presented in the Tab. 2, there were 519 individuals who were investigated through survey and 140 subjects have fulfilled the IBS Rome III criteria, while 109 and 31 met the Rome III criteria, but not the Rome IV, and met both the Rome III and IV criteria, respectively. Notably, 6 subjects reported to have the Rome IV but not the Rome III and due to data inconsistency, these 6 subjects were excluded and have not been included into consideration among those 140 identified IBS subjects. The reason for exclusion of these 6 subjects was due to inconsistency in answering the questions and as for the questions on the IBS Rome III criteria: they were unclear, which made them complex to understand and include them in the analysis. With that said, in Zrenjanin, IBS prevalence from the conducted survey was reported to be 26.97% (140 IBS positive out of 519 subjects) based on the Rome III criteria.
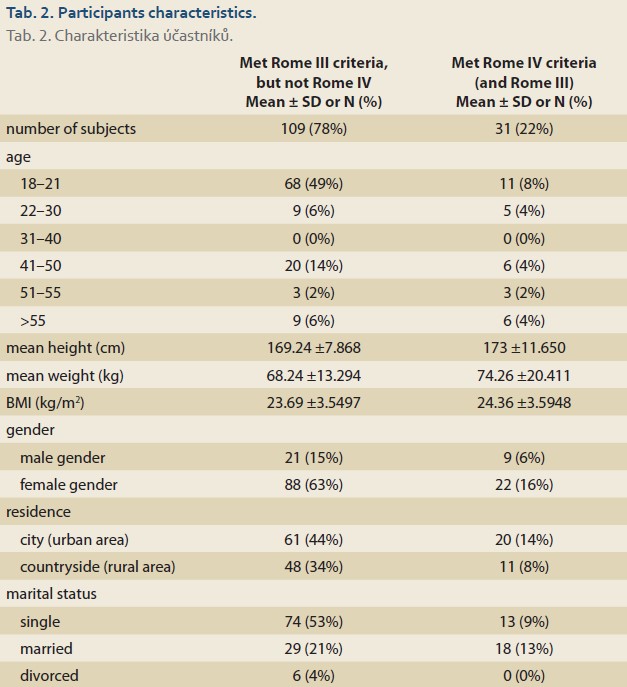
Overall, 110 subjects were female, and 30 were male. Within the Rome III subjects, the mean height and weight were 169.2 cm and 68.2 kg, respectively, and the mean body mass index (BMI) was 23.69 kg/m2, while among the Rome IV subjects’ height and weight were 173 cm and 74.2 kg, resulting into the mean BMI of 24.36 kg/m2. In total, 58% subjects lived in urban areas and 36% lived in rural areas. All in all, 62% subjects were single, and 34% were married, with a small number of the remaining subjects being divorced.
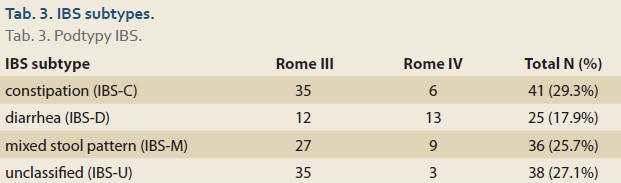
The IBS subtypes (based on the Rome III and IV criteria) were distributed as follows: 41 (29.3%) IBS-C, 25 (17.9%) IBS-D, 36 (25.7%) IBS-M and 38 (27.1%) IBS-U, presented in the Tab. 3.
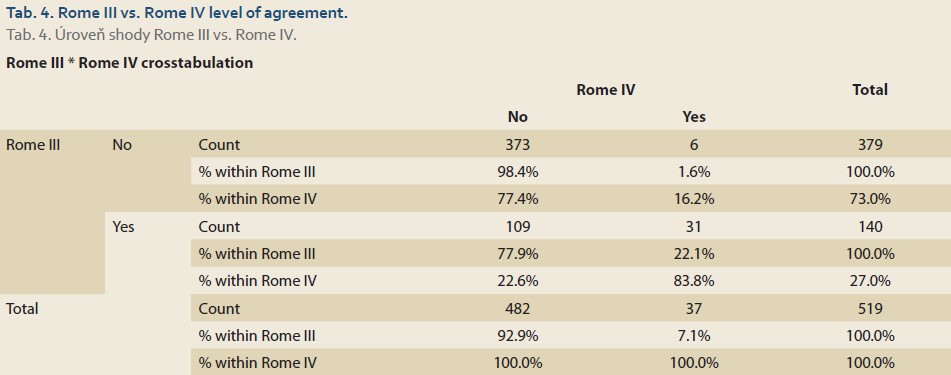
Proportion of individuals with irritable bowel syndrome meeting the Rome III and the Rome IV criteria and level of agreement
In total, out of 519 individuals with provided survey, 140 (26.97%) met the Rome III IBS diagnosis criteria. 37 (7.12%) met the Rome IV criteria for IBS. Among the 37 individuals meeting the Rome IV criteria for IBS, only 6 (16.22%) did not meet the Rome III criteria, as well. The kappa statistic for the level of agreement between the Rome III and the Rome IV was 0.268, indicating only moderate agreement closer to poor agreement margin (Tab. 4).
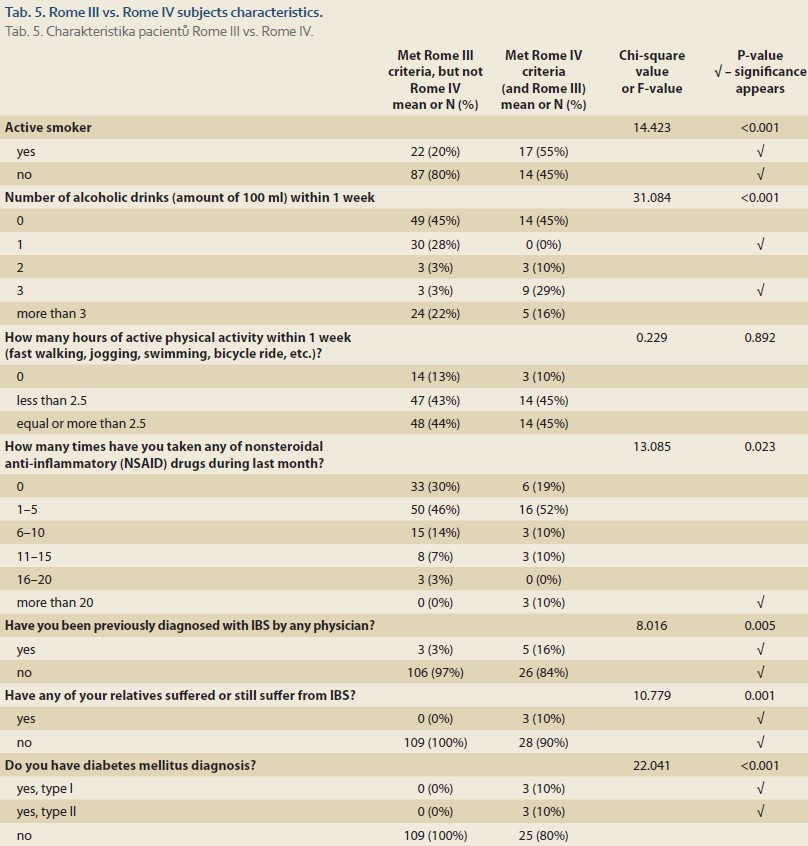
Comparison of the characteristics between the Rome III IBS subjects diagnosed with and without the Rome IV criteria
A significant difference has been noted in several investigated characteristics within the Rome III IBS diagnosed subjects between those with and without the Rome IV criteria. From the aspect of the subjects’ habits, there were more non-smokers among the Rome III without the Rome IV than with the Rome IV (P <0.001) (Tab. 5). Also, a significantly higher number was noted of the Rome III subjects without the Rome IV who drink alcohol moderately (100 ml per week) than with the Rome IV criteria (P <0.001) and much more patients with the Rome IV criteria drink alcohol more often (3 times of 100 ml per week) than without the Rome IV criteria (Tab. 5). This potentially indicates that the more frequent alcohol consumption develops, the more severe IBS symptoms, such as abdominal pain and other criteria that falls under the Rome IV criteria. No significant difference was noted in regard to physical activity among groups.
With regard to the medical history, the subjects with the Rome IV criteria were noted to be using much higher number (more than 20 drugs) of nonsteroidal anti-inflammatory (NSAID) drugs than the Rome III subjects. Nevertheless, both the Rome III and IV subjects have moderately (used 1–5-times over the last month) NSAID drugs, but without significant difference among these investigated groups (P = 0.023) (Tab. 5).
Furthermore, it was noted that more subjects with the Rome IV criteria have been previously diagnosed with IBS, 16% vs. 3%, respectively (P = 0.005). Also, a higher occurrence of relatives that suffered or still suffer from IBS in the Rome IV than the Rome III subjects, 10% vs. 0% respectively (P = 0.001) has been observed.
A certain number of subjects with the Rome IV criteria have reported to have either type 1 or 2 diabetes mellitus disease, while that was not the case with the Rome III subjects (P <0.001) (Tab. 5).
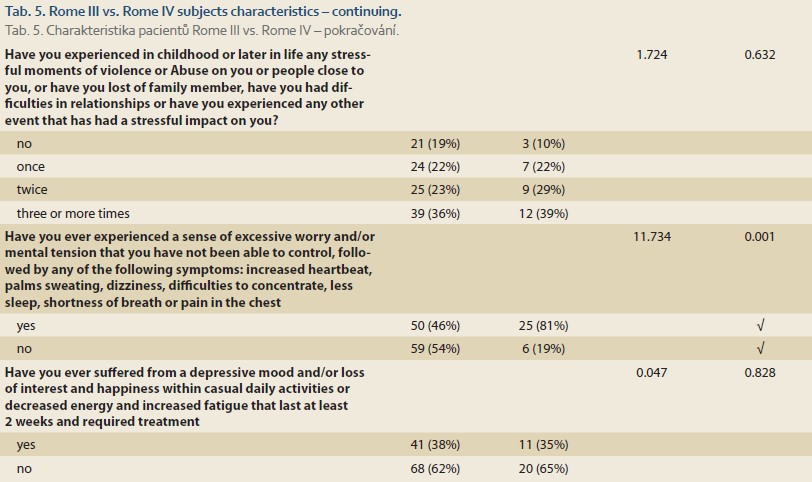
Last but not least, from the mental aspect i.e., those who suffer from a depressive mood or have experienced stressful moments in childhood or later in life, there were no significant differences between the Rome III and the Rome IV groups. Although it was noted with significant difference that almost all Rome IV subjects have experienced a sense of excessive worry and/or mental tension that they have not been able to control, compared to the Rome III subjects, where half of them experienced those symptoms (P = 0.001) (Tab. 5).
Discussion
Although epidemiology characteristics of IBS have been comprehensively investigated worldwide, in Serbia, the data for the IBS lack. IBS is a common chronic disorder affecting 9–23% of the population [13]. In the present paper, IBS prevalence from the conducted survey was reported to be 26.97% in the Central Banat District, a part of the northern region of Vojvodina. Notably, Vojvodina, as a part of Serbia, is adjacent to Croatia. In Croatia, a high prevalence of IBS, such as 28.2% [14] and even 29.2% [11] has been reported in various publications, as well. Therefore, our finding might be closer to reality and a true statement, though further investigation in broader population, is required for validation. Also, the agreement between the Rome III and the Rome IV criteria for diagnosing IBS was moderate, based on the finding of this research.
According to this study, IBS prevalence was significantly higher in the females and was associated with a younger age, i.e. a significant difference was noted in the age group of 18–21 between the Rome III (68 subjects) and the Rome IV (11 subjects). It is generally noted that the Rome III prevalence is higher among females than in males in many published articles. Our finding that IBS is more prevalent in younger women was also found by Keeley M Fairbrass et al, where it is stated that those with the IBS-type symptoms were younger, more likely to be females [15].
Most participants reported several coexisting bowel symptoms and the majority reported experiencing symptoms at least several times per month. Constipation (IBS-C) was the primary most prevalent symptom, followed by unclassified (IBS-U), mixed stool pattern (IBS-M) and less frequently reported was diarrhea (IBS-D).
Interestingly, there have been more Rome III non-smokers than Rome IV (P <0.001). Also, there were significantly more Rome III subjects that consume alcohol moderately (100 ml per week) than Rome IV subjects (P <0.001). Nonetheless, there were more Rome IV subjects that consume alcohol more frequently (3 times of 100 ml per week) than Rome III subjects (P <0.001). This potentially indicates that the more frequent alcohol consumption develops, the more severe IBS symptoms, such as abdominal pain and other symptoms, that fall under the Rome IV criteria. Interestingly, somewhat same results showing alcohol impact on IBS results were reported by Rajaa Chatila et al study in the Lebanese population, where a significant difference occurs and indicates that those who have ever been alcohol drinkers were twice as likely to have IBS than never-drinkers [16]. Another publication written by Kerryn W. Reding et al found that IBS symptoms differ according to the pattern of alcohol intake among IBS patients, suggesting that the pattern of drinking may in part explain the inconsistent findings between alcohol and IBS symptoms [17].
The Rome IV subjects have used excessive NSAID drugs (more than 20 NSAID drugs per month) while none of the Rome III subjects have exaggerated in NSAID drugs use, and a significant difference occurs in this comparison. This study has also shown that the most frequent use of NSAID drugs in both the Rome III and the Rome IV subjects has been noticed in moderate consumption but without statistical significance. Another study done by In Naif H. Alqahtani and Mohammad Eid M. Mahfouzfrom in Saudi Arabia showed that regular use of NSAIDs was significantly higher in IBS patients [18]. Nevertheless, further prospective cohort studies are needed to confirm NSAIDs as a risk factor for IBS and to help identify the etiological nature of this association.
Among the most common psychiatric symptoms, such as excessive worry and/or mental tension that they have not been able to control, appear to be more frequent in the Rome IV population (25, 81%) than in the Rome III (50, 46%) with significant difference of P = 0.001. Similar findings that present higher stress among the Rome IV population were reported in Christopher J. Black et al study [19]. Further studies should investigate the difference between the Rome III and the Rome IV frequency of psychiatric symptoms. Nevertheless, from the mental aspect i.e., suffering from depressive mood or experiencing stressful moments in childhood or later in life, there were no significant differences between the groups.
Notably, we have been investigating IBS epidemiology, although this was a questionnaire study on a population sample of unknown relevance, where an organic cause of symptoms has not been ruled out, so the diagnosis of IBS is not certain and the data may be overestimated. Nevertheless, due to the lack of epidemiology data in this region, this was one of the first studies that have determined the prevalence of IBS in healthy general population in Central Banat District, Serbia, by using the Rome III and IV criteria. Also, it further compared the characteristics among the Rome III and the Rome IV subjects. There were other limitations to this study as well. The risk factors for IBS were not identified and the association between the risk factors and the incidence of IBS could not be established at the moment between the Rome III and the Rome IV population.
Conclusion
In this study, the prevalence of IBS in Serbia is very high. The prevalence is higher among females than among males. The most prevalent subtype was IBS-C, followed by other subtypes. In this study, we have seen a correlation between smoking, alcohol and NSAID usage, and the early signs are showing that abuse of smoking, alcohol and NSAID led to more severe form of IBS, based on the Rome IV criteria. There were significant numbers of the Rome IV patients who were previously diagnosed with IBS syndrome and who had relatives with IBS. Last but not least, excessive worry and/or mental tension that they have not been able to control are shown to be more frequent in the Rome IV population.
After consideration of the abovementioned findings, it is recommended for young people to be screened for IBS. Any symptom of change in stool frequency or consistency should raise a suspicion of IBS after undergoing all the relevant investigations for ruling out organic diseases. This will aid their early diagnosis and will help to improve their quality of life. Furthermore, prevalence of IBS is significantly lower when the Rome IV criteria is used, due to restrictive criteria (like abdominal pain).
Understanding of the brain and gut axis disorders and improvements of diagnostic criteria, such as Rome IV, are providing a hope for better knowledge of the disease, more precise diagnostic and finding for a better treatment modality.
ORCID author
A. Preveden ORCID 0000-0003-3572-2604.
Submitted/Doručeno: 6. 3. 2022
Accepted/Přijato: 24. 8. 2022
Dusan Slankamenac, MD
Department of Gastroenterology
General Hospital
Ive Lole Ribara 38
230 00 Zrenjanin
Serbia
slankamenacdusan@gmail.com
To read this article in full, please register for free on this website.
Benefits for subscribers
Benefits for logged users
Literature
1. Whitehead WE, Validation Working Team Committee in association with the Rome Questionnaire C. Development and validation of the Rome III diagnostic questionnaire. In: Drossman DA, ed. Rome III: the functional gastrointestinal disorders. 3rd ed. McLean VA: Degnon Associates Inc., 2006: 835–853.
2. Sainsbury A, Sanders DS, Ford AC. Prevalence of irritable bowel syndrome-type symptoms in patients with celiac disease: a meta-analysis. Clin Gastroenterol Hepatol 2013; 11(4): 359.e1–365.e1. doi: 10.1016/j.cgh.2012.11.033.
3. Palsson OS, Whitehead WE, van Tilburg MA et al. Rome IV diagnostic questionnaires and tables for investigators and clinicians. Gastroenterology 2016; S0016-5085(16)00180-3. doi: 10.1053/j.gastro.2016.02.014.
4. Francis CY, Morris J, Whorwell PJ. The irritable bo- wel severity scoring system: a simple method of monitoring irritable bowel syndrome and its pro- gress. Aliment Pharmacol Ther 1997; 11(2): 395–402. doi: 10.1046/j.1365-2036.1997.142318000.x.
5. Wong R, Lee J, Fernandes M. Updates in gastrointestinal practice guidelines for the family physician. 2018 [online]. Dostupné z: https: //specialty.mims.com/topic/updates-in-gastrointestinal-practice-guidelines-for-the-family-physician.
6. Lovell RM, Ford AC. Global prevalence of and risk factors for irritable bowel syndrome: a meta-analysis. Clin Gastroenterol Hepatol 2012; 10(7): 712.e4–721.e4. doi: 10.1016/j.cgh.2012.02.029.
7. Hungin AP, Whorwell PJ, Tack J et al. The prevalence, patterns and impact of irritable bowel syndrome: an international survey of 40,000 subjects. Aliment Pharmacol Ther 2003; 17(5): 643–650. doi: 10.1046/j.1365-2036.2003.01456.x.
8. Drossman DA. The functional gastrointestinal disorders and the Rome III process. Gastroenterology 2006; 130(5): 1377–1390. doi: 10.1053/ j.gastro.2006.03.008.
9. Enck P, Aziz Q, Barbara G et al. Irritable bowel syndrome. Nat Rev Dis Primers 2016; 2: 16014. doi: 10.1038/nrdp.2016.14.
10. Kim JH, Lin E, Pimentel M. Biomarkers of Irritable Bowel Syndrome. J Neurogastroenterol Motil 2017; 23(1): 20–26. doi: 10.5056/jnm16135.
11. Oka P, Parr H, Barberio B et al. Global prevalence of irritable bowel syndrome according to Rome III or IV criteria: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol 2020; 5(10): 908–917. doi: 10.1016/S2468-1253(20)30217-X.
12. Keszthelyi D, Dackus GH, Masclee GM et al. Increased proton pump inhibitor and NSAID exposure in irritable bowel syndrome: results from a case-control study. BMC Gastroenterol 2012; 12: 121. doi: 10.1186/1471-230X-12-121.
13. Adriani A, Ribaldone DG, Astegiano M et al. Irritable bowel syndrome: the clinical approach. Panminerva Med 2018; 60(4): 213–222. doi: 10.23736/S0031-0808.18.03541-3.
14. Canavan C, West J, Card T. The epidemiology of irritable bowel syndrome. Clin Epidemiol 2014; 6: 71–80. doi: 10.2147/CLEP.S40245.
15. Fairbrass KM, Selinger CP, Gracie DJ et al. Prevalence and impact of Rome IV versus Rome III irritable bowel syndrome in patients with inflammatory bowel disease. Neurogastroenterol Motil 2022; 34(5): e14256. doi: 10.1111/ nmo.14256.
16. Chatila R, Merhi M, Hariri E et al. Irritable bowel syndrome: prevalence, risk factors in an adult Lebanese population. BMC Gastroenterol 2017; 17(1): 137. doi: 10.1186/s12876-017-0698-2.
17. Reding KW, Cain KC, Jarrett ME et al. Relationship between patterns of alcohol consumption and gastrointestinal symptoms among patients with irritable bowel syndrome. Am J Gastroenterol 2013; 108(2): 270–276. doi: 10.1038/ajg.2012.414.
18. Alqahtani NH, Mahfouz ME. The Prevalence and Risk Factors of Irritable Bowel Syndrome in Saudi Arabia in 2019. Int J Prev Med 2022; 13: 13. doi: 10.4103/ijpvm.IJPVM_ 486_20.
19. Black CJ, Yiannakou Y, Houghton LA et al. Epidemiological, Clinical, and Psychological Characteristics of Individuals with Self-reported Irritable Bowel Syndrome Based on the Rome IV vs Rome III Criteria. Clin Gastroenterol Hepatol 2020; 18(2): 392.e2–398.e2. doi: 10.1016/j.cgh.2019.05.037.